Abstract
Introduction:
Chronic Lymphocytic Leukemia (CLL) is frequently accompanied by immune dysregulation. Hypogammaglobulinemia is one of the most important immune defects encountered, and all three classes of immunoglobulins (IgG, A and M) can be involved. Recently, novel heavy+light chain (HLC) immunoassays have become available that quantify the light chain types of each immunoglobulin class (e.g. IgGk and IgGl). These assays are measured in pairs and provide information on the isotype produced by a tumour (the "involved" HLC), the non-clonal ("uninvolved") HLC, and the ratio (e.g. IgGk/IgGl) - which indicates monoclonality. HLC assays have been shown to improve monitoring of plasma cell dyscrasias, but their role in CLL is yet to be studied.
Methods
This is a multi-center study performed in collaboration with the Israeli CLL Study Group and involved 10 medical centers.
The cohort included 122 patients with CLL and 26 healthy controls. Baseline was defined as the time the blood sample was taken. Serum samples were analyzed for levels of IgG subclasses (IgG1, IgG2, IgG3, IgG4), heavy+light chains (HLC) (IgGκ, IgGλ, IgAκ, IgAλ, IgMκ or IgMλ) and free light chains (sFLC).
HLC-pair suppression was defined as an abnormal HLC ratio and uninvolved HLC levels below the normal reference range (i.e. in g/L: IgGκ<3.84; IgGλ<1.91; IgAκ<0.57; IgAλ<0.44; IgMκ<0.19; IgMλ<0.12).
HLC immunoparesis was defined as HLC isotype levels below the normal reference range, regardless of HLC ratio (i.e. HLC immunoparesis of at least 1 isotype indicates at least one of IgGκ, IgGλ, IgAκ, IgAλ, IgMκ or IgMλ below the normal reference range).
Severe HLC-pair suppression or severe HLC immunoparesis was defined as a concentration of the uninvolved HLC or any HLC isotype that is suppressed by >50% below the normal reference range. The association of variables with time to first treatment (TTT) was performed with Cox proportional hazard model.
Results
Current analysis was performed on 105 CLL patients who had complete data available; median age was 68 years, 64% were males and Binet stage A, B, C, were 80%, 18.1% and 1.9% respectively. Median time from diagnosis to baseline measurements was 27 months (range 0-328 months).
An abnormal sFLC ratio was identified in 70% (73/105) patients and summated k and λ concentrations (SFLC) were ≥70 mg/L in 18% of cases. An abnormal HLC ratio was present in 32% (34/105) patients, and 21% had HLC pair suppression of any 1 HLC isotype. HLC immunoparesis of 1, ≥2 and ≥3 isotypes was observed in 74 (70%), 58 (55%) and 36 (34%) of patients, respectively, with severe HLC immunoparesis identified in 40 patients (38%).
Patients with IgG2 suppression were more frequently hospitalized due to infection with an Odds Ratio of 3.826 (p=0.031).
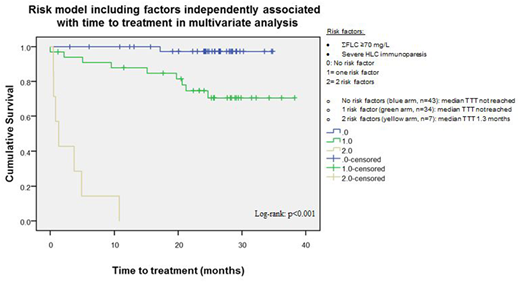
In multivariate analysis, SFLC ≥70 mg/L and severe HLC immunoparesis were independently associated with TTT (HR 15.3, p<0.001; HR 80, p<0.001 respectively). Using these 2 variables, a risk-stratification model was constructed that separated CLL patients into 3 risk groups (with 0, 1 or 2 risk factors) with significantly different TTT (p<0.001, Figure 1). Patients with both risk factors (SFLC ≥70 mg/L and severe HLC immunoparesis) had the shortest TTT.
Conclusions
The findings presented here demonstrate that there is considerable potential for the use of HLC and FLC immunoassays to provide prognostic information in CLL.
Tadmor:PFIEZER: Consultancy; JNJ: Consultancy; ABBVIE: Consultancy; NOVARTIS: Consultancy; ROCHE: Research Funding. Aviv:ABBVIE: Consultancy; ROCHE: Research Funding. Herishanu:ROCHE: Research Funding; JNJ: Consultancy; ABBVIE: Consultancy. Shvidel:ROCHE: Consultancy, Research Funding; ABBVIE: Consultancy, Research Funding; JNJ: Consultancy. Rahimi-Levene:ABBVIE: Consultancy. Ruchlemer:ABBVIE: Consultancy; JNJ: Consultancy. Fogl:The Binding Site Group Ltd: Employment. Polliack:ROCHE: Research Funding; ABBVIE: Consultancy. Magal:The Binding Site: Employment. Townsend:The Binding Site Group Ltd: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal